What to Do When Your Health Insurance Claim Is Denied
Quick Answer
If your health insurance claim is denied, it could be a simple error. Check your health insurance coverage details and call your doctor and insurance company for help. If your claim is still denied, you can file an appeal to have the decision reversed.
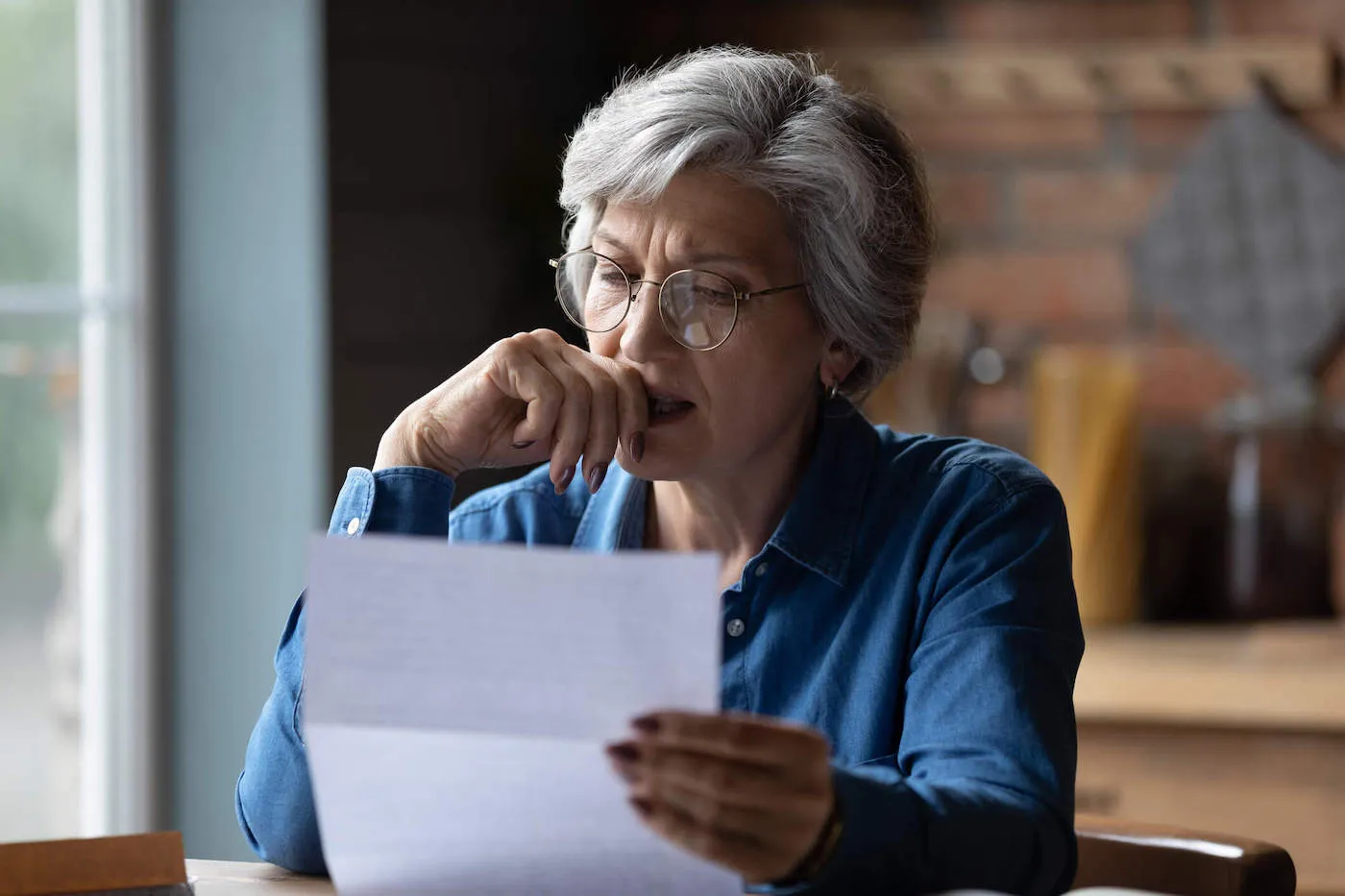
Discovering a pricey medical procedure isn't covered by your health insurance could be enough to cause a financial panic attack. If your health insurance claim is denied, review your health insurance policy's coverage carefully, contact the medical provider and insurance company to see whether there was an error and, if necessary, appeal the decision. Keep reading to learn what steps to take when your health insurance provider denies your claim.
Steps to Take When Your Health Insurance Claim Is Denied
1. Review Your Explanation of Benefits
By law, most health insurance plans must give you a written explanation of benefits (EOB) after a claim is filed. The EOB shows how much the insurance company paid and any remaining amount you owe. If the insurance company denies your claim, the EOB must explain why. Common reasons a claim is denied include:
- You went to an out-of-network provider.
- You didn't get precertification or preauthorization for a procedure.
- You haven't yet met your deductible.
- The service you received is not covered by your insurance.
2. Review Your Summary of Benefits and Coverage
Your summary of benefits and coverage (SBC) explains what benefits are covered and not covered. It also lists any deductible, copays or coinsurance you'll have to pay.
Still confused? Contact your health insurance company for clarification.
3. Check the No Surprises Act
Do you get health insurance through your job, Healthcare.gov, your state's marketplace or directly from an insurance company? The No Surprises Act may protect you from unexpected bills for health care received on or after January 1, 2022.
The act covers most emergency services and prevents providers from charging out-of-network cost sharing or billing you extra for services from non-network providers at an in-network facility. Check the details of the No Surprises Act to see if it covers your claim.
4. Contact Your Health Insurance Company
Still convinced your claim should have been covered? Often, claims are denied due to billing errors or missing information. Call your insurance company to see if this is the case. Have your health insurance card, the details of the visit (date, provider, reason, etc.) and the EOB handy when you call.
5. Contact Your Health Care Provider
If your health insurance company determines your claim was denied in error, they may contact your health care provider to settle the issue. Or you might need to be the go-between, calling both your provider and your insurer to get the problem resolved. Getting the two of them to talk to each other while you're on the line can speed things up.
6. Enlist Your Employer's HR Department
If, like many Americans, you get health insurance through your job, your employer pays the bulk of your premiums. They also have a vested interest in making sure you get the coverage they're paying for. When your efforts to work out the problem with the insurance company have stalled, your HR department may be willing to step in.
7. File an Internal Appeal With the Insurance Company
What if you've tried all the steps above and your insurance company still won't approve your claim? Under the Affordable Care Act (ACA), non-grandfathered group health insurance plans and carriers selling insurance to group and individual markets must allow consumers to file appeals when claims are denied. Contact your insurance company to learn the process for filing an internal appeal and whether there is a deadline to file.
Gather your documentation. Typically, you'll need to:
- Resubmit the claim.
- Provide the EOB denying the claim.
- Get a letter from your doctor explaining why the treatment, procedure or medication was or is medically necessary. Provide any supporting documents such as test results or medical records.
The National Association of Insurance Commissioners (NAIC) has a sample letter you can use to request an internal review.
Make a note to follow up with the insurer if you don't hear from them. Usually, insurers must complete internal reviews in the following time frames:
- Claims for urgent care: Within 72 hours
- Claims for treatment not yet received: Within 30 days. You can also request an expedited review if the situation is urgent—for example, your doctor says you need surgery right away.
- Claims for treatment you have received: Within 60 days
For insurance through Medicare or Medicaid, appeals follow different procedures.
- Call 800-MEDICARE for free help filing a Medicare appeal.
- Contact your state Medicaid agency for help filing a Medicaid appeal.
8. File an External Appeal
If the insurance company denies your internal appeal, you have the right to file an external appeal. An independent review organization will review your claim and make a final decision. The insurance company must abide by this decision.
You can file an external appeal if:
- The denial involves a medical decision where your health care provider disagrees with the insurance company.
- The denial involves a treatment that the insurer says is experimental or investigational.
Your EOB or most recent denial of your claim will tell you how to contact the independent review organization to file an appeal.
Tips to Help Get Your Health Insurance Claim Approved
To boost your odds of getting a claim approved:
- Keep detailed records. Whenever you contact anyone involved, write down:
- The date of the call, email or letter
- The name of the person you spoke to or wrote to
- What was said or the response you received
- Save all necessary documents. These include:
- Records of medical treatment or visits
- Receipts for copays or coinsurance
- Bills
- Any correspondence with the medical provider or insurance company
- Get help. Dealing with health insurance claims can get complicated. The following organizations can help.
- Consumer Assistance Program (CAP): Available in many states, these offices can answer questions about your health insurance or help you file an appeal. They may provide services by phone, email or in person.
- State Insurance Commissioner's Office: Insurance commissioners in each state assist consumers with insurance problems.
How to Pay for Medical Costs When Your Claim Is Denied
A big medical bill seems intimidating, but there are several ways to make it more affordable.
- Negotiate the charges or payment terms. Health care facilities or providers may be willing to reduce your overall bill or split it into monthly payments. Depending on your income, you may qualify for income-driven hardship repayment plans.
- Get help from nonprofit organizations. Organizations that help pay for care or medications include the HealthWell Foundation, the Leukemia & Lymphoma Society, the Patient Access Network Foundation and CancerCare. Local religious organizations may also provide aid.
- Look for pharmaceutical company patient assistance programs to help pay for medications. This can be especially helpful if you're on Medicare and your medications aren't covered by your Part A or Part B plans.
Understand Your Health Insurance
An ounce of prevention is worth a pound of cure when it comes to health insurance claims. To help ensure your health insurance claims are approved:
- Read your policy to determine what's covered.
- Understand how much the insurance company pays and what your responsibility is.
- Use in-network health care providers whenever possible.
- Obtain necessary preapprovals before getting health care.
Following your health insurance policy's rules can prevent an unexpected medical bill. By managing your health care costs, you'll keep your bank account in good health too.
What makes a good credit score?
Learn what it takes to achieve a good credit score. Review your FICO® Score for free and see what’s helping and hurting your score.
Get your FICO® ScoreNo credit card required
About the author
Karen Axelton is Experian’s in-house senior personal finance writer. She has over 20 years of experience as a journalist and has written or ghostwritten content for a variety of financial services companies.
Read more from Karen