Denial Management
Denial management solutions to improve cash flow
Are denied, suspended, pending or lost claims impeding your financial performance?
We know that denials management can often be manual and time consuming, ultimately leading to disappointing results.
With the right denial analysis and automation, healthcare organizations like yours can manage denials effectively and increase reimbursements significantly.
Denial Workflow Manager integrates the power of workflow, enhanced claim status, remittance detail, and analytics to optimize follow-up activities. You can identify denials, holds, suspends, zero pays, as well as appeals won or lost with payers through a combination of Electronic Remittance Advice (ERA) and enhanced claim status transactions.
Optimize claims follow-up by identifying and targeting the claims that need attention as quickly as possible.
Ready to lower denial rates?
Hear from our customers
Learn how Schneck Medical Center gained visibility into their denials in real time and can now proactively prevent denials.
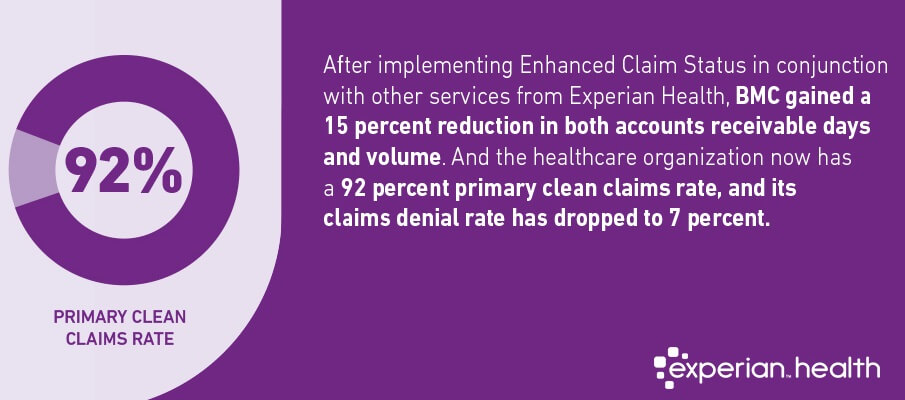
How Summit Medical Group Oregon decreased denials to achieve a 92% primary clean claim rate
Case study
Maximize reimbursements
Quickly identify denied claims that can be resubmitted and/or appealed.
Automate denials process
Eliminate the need for manual review of claims status and remittance advices.
Denials best practices
Standardize activity and root cause templates by denial types.
Identify trends
Determine root causes for denials to inform improved procedures.
Analysis and reporting
Extensive data analysis and reporting capabilities, allowing you to prevent denials in upstream processes.
Download product sheet
Standalone or integrated
Can be used as standalone product, or integrated with Experian ClaimSource to align claims and denials information on the same screens.
Customizable
Work lists generated based on client specifications, such as denial category and dollar amount.
Analytics
Access standard product reports, analytics reports, and forward responses to HIS/PMS systems.
ANSI reason codes
Provides ANSI reason codes and payer proprietary codes as well as descriptions.
ClaimSource®
ClaimSource® provides the workflow and automation you need to prioritize claims that need attention and minimize financial impact.
Contract Manager and Contract Analysis
Verify the accuracy of payment received from third-party payers.
Enhanced Claim Status
Enhanced Claim Status allows you to accelerate follow-up and improve cash flow.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.