
In July this year, the Centers for Medicare & Medicaid Services (CMS) reported that a data breach in a contractor’s network may have compromised the data of more than 600,000 current Medicare beneficiaries. The breach, which occurred in May 2023, involved a vulnerability in file transfer software that enabled an unauthorized party to access beneficiaries’ personally identifiable information (PII) and protected health information (PHI). Some patients were issued with new Medicare Beneficiary Identifiers (MBIs) following the incident. The contractor also offered two years of Experian credit monitoring at no cost to those affected. However, providers may see an increase in patients who are confused or concerned about using their MBI card. Experian Health’s MBI Lookup service can help providers ensure that Medicare eligibility verification remains as efficient as possible.
Thousands of beneficiaries issued new MBI numbers
In response to the breach, CMS announced that 47,000 individuals would be mailed new MBI cards with new MBI numbers. However, as 612,000 patients were affected by the breach, there may be a significant number of people whose MBIs may change without notice. Since these individuals will not be able to use their old MBIs when trying to find Medicare coverage and benefits, there could be confusion among patients and providers who rely on MBIs to confirm a patient’s eligibility for Medicare coverage. It could also affect billing processes and claim status inquiries.
Experian Health reached out to CMS for clarification and received the following guidance:
- If a Medicare beneficiary’s MBI number has changed, then their old (now inactive) MBI will return an AAA72 error when attempts are made to confirm coverage using the HIPAA Eligibility Transaction System (HETS).
- The HETS 270/271 platform will accept historical 270 requests that use the patient’s new MBI. Old MBI numbers will only be accepted if that number was active during the Date(s) of Service noted on the request.
Providers should note that some patients may inadvertently use invalid MBI numbers and review processes for verifying Medicare eligibility accordingly.
Verifying Medicare eligibility with Experian Health’s MBI Lookup tool
Verifying active coverage can be a painstaking process, but it’s a vital step to confirm that planned services will be covered by the patient’s insurance provider. If a patient is unaware or cannot demonstrate eligibility for Medicare, then the provider cannot make a claim for reimbursement, and the patient may be left to pay a bill they cannot afford. Finding active coverage helps providers reduce the risk of bad debt.
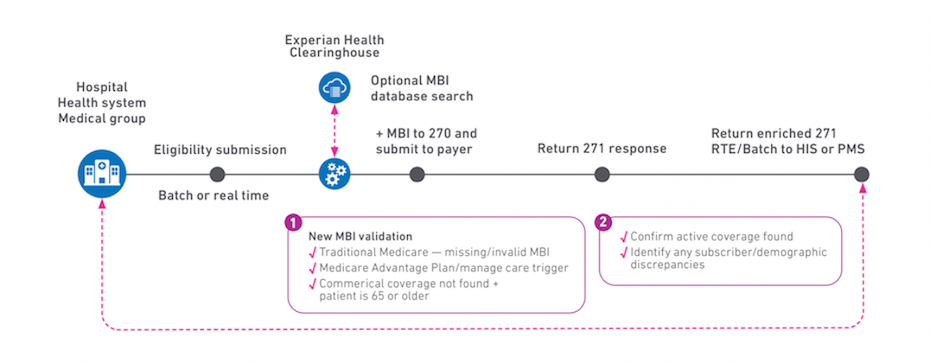
Experian Health’s Insurance Eligibility Verification speeds up this process by accurately confirming coverage at the time of service. The process comes with an optional MBI Lookup feature, which checks transactions against MBI databases to see if the patient may be eligible for Medicare. If the patient has forgotten their MBI card, the tool will check to see if they’re included in the database, using their name, date of birth, and Social Security Number (SSN) or Health Insurance Claim Number (HICN).
The MBI Lookup service triggers on 270/271 transactions in the following cases:
- Where the transaction fails because the subscriber is not found or their MBI number or other identification is missing or invalid (a “Traditional Medicare Failure”)
- Where a commercial 270 inquiry returns a “Medicare Advantage Plan” or “Managed Care Plan” indication on the “Other Payer” or “Other Coverage” section of the 271 response
- Where a commercial 270 transaction returns a failed response and the patient is aged 65 or older.
If the provider’s system attempts to use a patient’s old number, and the patient does not realize that they have a new number or card, MBI Lookup will find and verify their new MBI. When the tool is triggered, it finds active and verified MBI numbers in 60% of cases on average.
Find coverage faster with automated discovery tools
Kate Ankumah, Principal Product Manager of Eligibility Verification and Alerts at Experian Health, says the automated MBI Lookup service has proven especially useful during times of change:
“Providers relied on this service to verify Medicare coverage quickly when the pandemic hit, just as the industry was adjusting to the use of MBIs instead of their legacy HICN. Now, MBI Lookup can help providers smooth out the impact of data breaches involving Medicare beneficiaries with minimal fuss. It’s a reliable way to give patients clarity without placing any undue burden on staff.”
Insurance Eligibility Verification can be used alongside other automated coverage identification tools, such as Coverage Discovery®. Coverage Discovery scans government and commercial payer databases throughout the patient journey to find any previously unknown or forgotten coverage, eliminating the need for manual inquiries. Using multiple sources of data and tried-and-tested algorithms, these tools work together to locate coverage for patients, giving patients peace of mind and helping providers avoid uncompensated care. Both tools can be accessed via the eCareNext® platform, so staff can view eligibility responses and manage work queues through a single interface.
And of course, this recent breach is a stark reminder of the need to protect patient data. Using a single vendor with integrated software and data solutions can help reduce the risk of data getting into the wrong hands.
Find out more about how Experian Health’s Eligibility Verification solution and MBI Lookup tool can help providers verify active coverage and give patients peace of mind following a data breach.


