Experian Health Blog
Learn how improving insurance eligibility verification at the early stages of the patient journey can help increase cash flow and reduce denials.

On April 1, 2023, millions of Medicaid recipients are set to lose coverage as the U.S. government’s COVID-19 public health emergency (PHE) expires. The Kaiser Family Foundation estimates that 5.3 to 14.2 million people will lose Medicaid coverage as the continuous enrollment provision of the PHE ends. Of this group, 6.8 million may be eligible to re-apply for Medicaid, but in the immediate term, it falls to patients and providers to sort through coverage questions, navigate charity and Medicaid eligibility, and keep bills out of collections. Mindy Pankoke, Senior Product Manager at Experian Health, shares her insights on how Patient Financial Clearance and other digital solutions can help providers and patients cut through the confusion to achieve the best healthcare and financial outcomes during this time. Q1: The public health emergency is ending on April 1, which means that many will lose Medicaid coverage. How will this impact providers and patients? “Patients who qualified for Medicaid under the Public Health Emergency requirements during COVID will be dropped from Medicaid on April 1, leaving them without coverage,” explains Pankoke. “Healthcare organizations have been trying to reach out proactively to pre-enroll some of these patients, but others may not know what their options are or may show up to receive care without realizing they no longer have coverage.” Patients will face a range of financial challenges. “Self-pay patients may defer treatment, which could keep them from receiving the care they need and may ultimately lead to more costly hospital visits,” Pankoke says. “Also, patients may be confused about what’s happened to their coverage and what their options might be going forward. If they end up being responsible for paying out of pocket for care, some may have to choose between paying their medical bills and paying for food or utilities.” Providers will see a surge in patients needing help after losing Medicaid coverage With millions of patients in flux, providers will need to dedicate time and attention to helping patients sort through their concerns, including: Confirming whether Medicaid coverage is still in force Verifying coverage with new insurance Determining eligibility to re-enroll in Medicaid Qualifying patients for full or partial charity care Explaining patient financial responsibility and working out payment plans Managing billing and collections with a higher volume of accounts in AR Optimizing outcomes so that patients get the best care possible and providers end up with the least amount of bad debt Time is a critical element. Lengthy processes and administrative delays are likely to increase patient stress levels. Meanwhile, many providers face industry-wide staffing shortages. Time-consuming manual processes, multiplied by a sudden surge of affected patients, could quickly become overwhelming for staff. “For providers, this could be a hard situation to navigate,” says Pankoke. “At the same time, it gives providers an opportunity to come through for patients in a moment of need. Being able to identify patients who need assistance and offering them help can be powerful.” Q2: That raises an important question: How can providers create a compassionate experience for patients? “I think awareness is one place to start: making sure your staff knows this change is coming and that they understand the impact,” Pankoke says. “Your staff are the ones who’ll be working with patients personally when they come in and find out they no longer have Medicaid coverage.” But compassion doesn’t end there. “Many providers already have charity programs in place to provide relief for patients who can’t afford care,” says Pankoke. “The challenge lies in identifying the patients who need that charity assistance and connecting them to the help that’s available, while also learning which patients may still qualify for Medicaid and need help to re-enroll. Patient Financial Clearance uses credit and non-credit data to identify patients who may still be eligible for Medicaid, as well as self-pay patients who may qualify for charity assistance.” Using data-driven digital tools to quickly and proactively size up patient financial needs and offer personalized help can make the patient experience more humane. “Making these steps easier is another piece of being compassionate.” Q3: Screening for charity can be complicated, especially when new regulations are introduced – how do providers streamline this process? “My best advice is to embrace your charity programs and use a partner like Experian Health to help you automate the financial assistance screening process,” says Pankoke. “Patient Financial Clearance removes the manual screening for the likelihood to qualify for your charity programs and Medicaid. It can automate the document-gathering in a patient-friendly way, and speed up the process to extend charity assistance, or work to enroll those likely to qualify for Medicaid early on before patients go through a costly uncollectable experience.” Automating these processes doesn’t have to be onerous. “Clients can provide their charity policy requirements to Experian Health and let our expert consultants help to create the most effective and efficient workflows for Medicaid and charity screening both up-front and as back-end scrubs.” Pankoke also urges providers to consider patient self-screening options as well: “Providers should consider other options aside from paper applications. We’ve seen clients shrink the application process from 60 days of paperwork down to 3.5 days by enabling patient self-screening options via text. This creates a better experience for the patient and hospital staff.” Q4: What else can providers do to help patients manage the cost of care? Providers can focus their resources on improving the patient's financial journey—for all patients, not just those who are struggling with their Medicaid status. Pankoke’s suggestions: Reach patients on their preferred channels – “Providers can empower patients with less paper-heavy ways to apply for financial assistance. Text and online applications embedded on your website or patient portal put the power into the patient’s hands using the channels they prefer.” Providers can also offer patients the ability to make payments right from their mobile devices using Patient Financial Advisor, making it easier to pay outstanding bills anytime and anywhere. Use data to gain insight into patient finances and offer personalized options – “In addition to screening for possible charity and Medicaid eligibility, Experian data enables providers to offer realistic payment plan options that consider how much the patient is likely to afford, enabling patients to bite off what they can chew with higher likelihoods of making payments successfully.” Customize collections – Sending patients who are struggling to collections may not be cost-effective or compassionate. “Providers don’t want to hound people for payment if the patient is having trouble covering their basic expenses and could qualify for Medicaid or charity care,” says Pankoke. Using Collections Optimization Manager, providers can tailor collections processes to their own specific needs. “A partner who is agnostic to your in-house and early-out agencies can help you manage, monitor, and optimize agency performance for maximum revenue.” Providers who are concerned about upcoming shifts to Medicaid coverage may want to consider leveraging solutions like Patient Financial Clearance, Collections Optimization Manager and Patient Financial Advisor to help them meet this challenge—along with the many challenges of managing patient financial needs in a rapidly-changing world.

Learn how Schneck Medical Center leveraged AI Advantage™ to help their organization reduce claim denials and maximize reimbursements.

Learn how self-scheduling helps reduce healthcare staffing challenges by making it easier for patients to access care and prepare for visits.

Clear, convenient and compassionate – patient-friendly billing should check off all three. But how many patients see this in practice? For many, the healthcare billing and payment process can be intimidating, confusing and rooted in paper-based systems that are slow and prone to error. With the right technology, providers can improve the billing experience by making it easier for patients to understand their financial responsibility and plan their payments. Online patient payment software can streamline the billing process by giving patients more flexibility and control. Here are 5 patient-friendly billing practices that providers can implement to improve the patient experience and protect revenue: 1. Provide proactive and reliable cost estimates Patients don’t want to feel like they’re in the dark when it comes to figuring out their financial responsibility. Unfortunately, too many receive no upfront estimates of the cost of care or receive estimates that aren’t accurate. This financial uncertainty can have a knock-on effect on patient care and provider cash flow. A survey by Experian Health and PYMNTS found that 46% of patients had canceled care after receiving a high-cost estimate, while 60% of patients with out-of-pocket expenses said they would consider switching providers after receiving inaccurate estimates. Patient Payment Estimates generates accurate, personalized estimates for each patient before and at the point of service. The patient’s liability is clearly broken down so they know exactly what to expect. Patients feel more in control and can make quicker, better decisions about how and when to pay (including paying upfront if they wish). This tool also helps providers comply with the Hospital Price Transparency Rule. 2. Eliminate confusing billing information In the age of Amazon, patients expect billing information to be clear, accessible and provided through their preferred channel. Long paper statements sent by mail or a single phone number to call during limited office hours likely won’t cut it. Providers should consider a multichannel approach that uses relevant patient financial data and consumer preferences to deliver personalized options. PatientSimple® is a self-service payments portal that allows patients to view statements online, generate pricing plans and manage their bills, all from a single dashboard. Patients can get automated email reminders and even pay in full. When patients have all the information they need at their fingertips, providers can spend less time handling queries and chasing payments. 3. Find missing coverage early Another ingredient in patient-friendly billing is to help patients reduce their liability, by tracking down any insurance coverage that might have been forgotten. Many patients relocated or changed employers during the pandemic, leaving many unclear about their current coverage. They may be misclassified as self-pay or assumed to have only one form of insurance. Coverage Discovery automatically checks for any active coverage that may have been missed. In 2021, Coverage Discovery tracked down previously unknown billable insurance coverage in more than 27.5% of self-pay accounts, finding over $66 billion in corresponding charges. This greatly reduces the financial burden on patients, while increasing reimbursement rates for providers. It’s just one example of a non-patient-facing tool that works behind the scenes to streamline patient collections. Discover how Stanford Health Care collaborated with Experian Health to optimize collections and improve the patient experience with Coverage Discovery and Collections Optimization Manager. 4. Patient-friendly billing requires personalized payment plans When it comes to payment, some patients will prefer to pay upfront and in full, while others want or need to spread out the cost into more manageable chunks. Providers can pull together financial, demographic and consumer data to point patients toward the right pathway. This is how Patient Financial Clearance works: patients are guided to a payment plan that makes the most sense for their individual situation, with a clear breakdown of what they’ll need to pay and when. Patients are automatically screened for financial assistance programs and can fill out applications online. 5. Allow convenient and flexible ways to pay Patients want simple and easy ways to pay. They expect a choice of quick and convenient digital payment methods that can be accessed anytime, anywhere. The preference for digital payment solutions is especially apparent among younger generations. More than half of millennials say they’re “very” or “extremely” interested in digital services. With online patient payment software, patients have the option to pay multiple providers at once, using multiple forms of digital payments. They can store credit card information on file or set up a digital wallet, and set up automatic recurring payments to stay on track. Offering secure, flexible and instant payment methods to patients from the start of their healthcare journey increases the chance of prompt payment. Patients are free to focus on their health, while providers will see an increase in cash flow with less time spent on collections. Patient-friendly billing practices create better patient experiences Outdated patient portals, poor communication and clunky billing processes do not make for a patient-friendly financial experience. The good news for providers (and their patients) is the growing menu of digital tools to offer patients the clarity and flexibility they expect. Experian Health President Tom Cox says: “Payment options are increasingly digital and more convenient, payment plans are more common, and price estimates have become less of a rarity. There is also greater use of non-clinical data to get a broader view of patients and their unique financial solutions. Data, coupled with the right technology, can help providers make sense of it all and enhance the patient journey.” Find out more about how Experian Health’s online patient payment software can help healthcare organizations build a modern financial experience to benefit patients and providers.

Medicaid continuous enrollment will come to an end on March 31, 2023, as the temporary provisions are decoupled from the COVID-19 public health emergency. The federal government introduced the protections to ensure individuals did not lose coverage during the pandemic, leading to record enrollment levels. But as states prepare to resume routine renewals, up to 15 million people could end up without adequate insurance. Coverage gaps could disrupt access to health services and increase the risk of uncompensated care for providers. With Medicaid continuous enrollment coming to an end, how can providers prepare? Mitigating the effects of the unwinding of the Medicaid continuous enrollment provision Under the Consolidated Appropriations Act passed in December 2022, states will have 14 months to complete renewal processes for Medicaid and the Children’s Health Insurance Program (CHIP). While 6.8 million people are likely to remain eligible, churn and administrative delays could leave some without coverage. Analysis by the Kaiser Family Foundation suggests that in recent years, around 65% of people who disenroll from Medicaid or CHIP experience a gap in coverage for all or part of the following 12 months. Some transition to other forms of coverage, but around 41% eventually re-enroll. Implementation of the forthcoming “unwinding” process largely falls to states. While the new legislation and associated guidance bring welcome certainty, concerns remain around how to avoid unnecessary disenrollment and expedite redetermination. That way, patients (and providers) aren’t left holding bills that could have been covered when the Medicaid continuous enrollment period ends. 4 things providers can do if a patient loses Medicaid coverage As patients steel themselves for the return of renewal paperwork, providers are considering how they can help patients maintain coverage and get the financial assistance they need. Digital self-service tools to apply for financial assistance can help patients access the appropriate support, with tailored payment plan options based on their individual financial situation – all through automation. Here are 4 key actions for providers to consider: 1. Find missing coverage with Coverage Discovery Healthcare providers should put automated processes in place to find any active coverage that may have been overlooked. Coverage Discovery searches for any billable government or commercial insurance to eliminate unnecessary write-offs and give patients peace of mind. Using advanced search heuristics, millions of data points and powerful confidence scoring, this tool checks for coverage across the entire patient journey. If the patient’s status changes, their bill won’t be sent to the wrong place. In 2021, Coverage Discovery identified previously unknown billable coverage in more than 27.5% of self-pay accounts, preventing billions of dollars from being written off. 2. Quickly identify patients who may be eligible for Medicaid and financial assistance A lack of clarity around enrollment and eligibility could cause chaos for claims and collections teams. How can they handle reimbursements and billing efficiently if financial responsibility is unclear? Claim denial rates are already a top concern for providers, on top of wasted time from seeking Medicaid reimbursement for disenrolled patients. Equally, patient collections will take a hit if accounts are designated as self-pay when the patient is entitled to financial assistance and charity care. It may be difficult to tell who’s who without a robust process to check patients’ ability and propensity to pay. With Patient Financial Clearance, providers can quickly determine if patients are likely to qualify for financial support, then assign them to the right financial pathway, using pre- and post-service checks. Self-pay patients can be screened for Medicaid eligibility before treatment or at the point of service, and then routed to the Medicaid Enrollment team or auto-enrolled as charity care if appropriate. Post-visit, the tool evaluates payment risk to determine the most suitable collection policy for those with an amount to pay and can set up customized payment plans based on the patient’s ability to pay. Patient Financial Clearance also runs back-end checks to catch patients who have already been sent a bill but may qualify for Medicaid or provider charity programs. This helps providers secure reimbursement and means patients are less likely to be chased for bills they can’t pay. 3. Screen and segment patients according to their propensity to pay Optimizing collections processes is always a smart move for providers, and will be particularly important when federal support ends. Collections Optimization Manager uses advanced analytics to segment patient accounts based on propensity to pay and send them to the appropriate collections team. With access to Experian’s consumer credit data, the Collections Optimization Manager segmentation models are powered by a more unique and more catered approach that includes robust and proprietary algorithms. It screens out Medicaid and charity eligibility, so collections staff focus their time on the right accounts. Between 2019-20 and 2020-21, UCSDH increased collections from around $6 million to over $21 million with Collections Optimization Manager. Altru Health System also used this solution to ensure that patients who were eligible for Medicaid were not allocated to collections and their insurance was billed promptly. Over a 10-month period, more than 4,000 accounts were flagged as eligible for financial assistance, representing nearly $2.7 million. This automated process also alleviates the burden on staff, who will likely be handling greater numbers of queries from anxious patients when continuous enrollment ends. 4. Make it simpler for patients to manage and pay bills The reality is that many patients affected by the unwinding of continuous enrollment will be on low incomes. When more than half of patients say they’d struggle to pay an unexpected medical bill of $500, providers need to take steps to make it easier for patients to gauge their upcoming bills. Digital, self-service tools such as Patient Financial Clearance can help self-screen for charity and financial assistance. Patient Financial Advisor and PatientSimple can help patients navigate the payment process with pre-service estimates, access to payment plans and convenient payment methods they can access on a computer or mobile device. Together, these tools can help providers manage the fluctuating Medicaid continuous enrollment landscape efficiently and offer extra support to patients who may be facing disenrollment. Find out more about how Patient Financial Clearance and other digital solutions can help healthcare organizations deliver compassionate financial experiences to their patients.

Discover how Stanford Health Care collaborated with Experian Health to optimize collections and improve the patient experience.

Dive into the world of AI and machine learning for healthcare with our new infographic, and learn how these tools are utilized.

Find out how online payment software can help healthcare organization increase collections and improve patient satisfaction.

Discover how UCSDH collaborated with Experian Health to improve patient billing, increase collections and reduce bad debt.

Healthcare providers are under increasing pressure to improve the patient experience. Here are three ways they can do it in 2023.
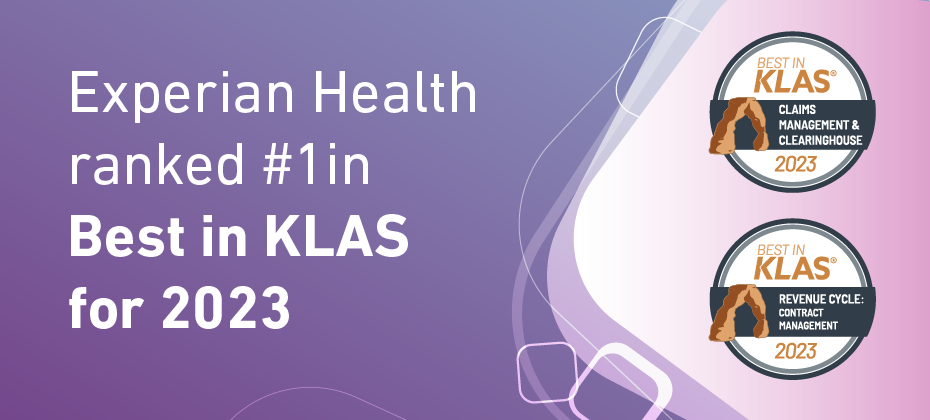
Experian Health is very pleased to announce that it ranked #1 in Best in KLAS, Software and Professional Services, for two segments: #1 in Claims Management and Clearinghouse, for our ClaimSource® claims management system #1 in Revenue Cycle, Contract Management, for our Contract Manager and Contract Analysis product. According to KLAS CEO Adam Gale, “The 2023 Best in KLAS report highlights the top-performing healthcare IT solutions as determined by extensive evaluations and conversations with thousands of healthcare providers. These distinguished winners have demonstrated exceptional dedication to improving and innovating the industry, and their efforts are recognized through their inclusion in this report. Congratulations to all the winning vendors for setting the bar for excellence in healthcare IT! KLAS continues to be committed to creating transparency and helping providers make informed decisions through our accurate, honest, and impartial reporting.” Experian Health’s 2022 State of Claims survey reveals that 47% of providers said that improving clean claims rates was one of their top pain points, with 42% reporting that denials have increased in the past year. Read how Hattiesburg Clinic in Mississippi, which uses both Contract Manager and Analysis and ClaimSource, leverages ClaimSource to automate claims management and reduce denials. Learn more about how ClaimSource and Contract Manager and Contract Analysis can help your healthcare organization.