Claims & Contract Management
Improve financial performance with automated, clean and data-driven medical claims management.
Artificial intelligence (AI) is changing the healthcare industry. From disease detection to chatbots, AI is having a significant impact on the way healthcare providers operate and deliver care to patients. Additionally, AI is transforming the revenue cycle management process by automating tasks, such as claim denials management. By leveraging AI tools, healthcare providers can reduce the time and resources required for manual claims processing, ensuring that claims are paid faster and with greater accuracy. As claim denials continue to rise by 10-15%, healthcare organizations continue to grapple with the adverse effects on their finances. That's why Experian Health created AI Advantage™ – an innovative solution that helps providers with better claim denial management. The first component, AI Advantage – Predictive Denials, proactively identifies claims that are at high risk of being denied, so providers can edit the claim prior to submission. The second component, AI Advantage – Denial Triage, steps in after claims have been denied to identify those with the highest potential for reimbursement. Schneck Medical Center is one example of a healthcare organization that has seen significant results from implementing AI Advantage. After just six months, they successfully reduced denials by an average of 4.6% each month. Corrections that would previously have taken their organization 12 to 15 minutes to rework could now be processed in under 5 minutes. With AI Advantage, healthcare organizations can improve their claim denials management processes, increase efficiency, and reduce administrative costs. The solution's ability to prevent and reduce claim denials in real time can help healthcare providers maximize revenue while delivering high-quality patient care. As healthcare organizations continue to face mounting financial pressures and staffing shortages, AI-powered solutions will be increasingly important in helping them navigate these challenges and achieve long-term success. Learn more about how healthcare organizations can begin their journey towards improving efficiency and reducing claim denials with AI Advantage.
Because so many healthcare claim denials originate in the front end of the revenue cycle, providers should focus on improving insurance eligibility verification at the early stages of the patient journey. Verifying coverage earlier in the billing process with automated eligibility verification software increases the chance of submitting clean claims the first time and protecting future revenue. As coverage and benefits become more challenging for patients to navigate, prioritizing eligibility could also hold the key to better patient-provider relationships. Given the complexity of the healthcare billing system, patients have little tolerance for errors and delays. Many already worry about being able to cover their financial obligations, so denied claims are the last thing they want to see. Insurance verification reduces denials, gives patients greater clarity over their upcoming expenses and allows healthcare organizations to focus on providing the best possible care. This article looks at why improving insurance eligibility verification can help healthcare providers optimize cash flow and achieve higher levels of patient satisfaction and loyalty. What are the steps in the insurance eligibility verification process? Before filling out a claim, providers must be sure that the services they’re seeking reimbursement for are covered by the patient’s health insurance. They must also check that the patient’s details match those on their insurance plan. If a provider offers treatment or services and it later turns out that the patient’s coverage has expired or the patient is ineligible for those items, the claim will be rejected. To verify eligibility, providers must therefore be able to answer the following questions: Are the patient’s contact details current and correct? Does the patient’s insurance plan cover the planned treatment or services? Do any exclusions apply under the patient’s plan? Have all necessary pre-authorizations been obtained? Is the coverage active? What are the thresholds for deductibles, co-pays or coinsurance, and do any annual or lifetime limits apply? Confirming eligibility early on lays the groundwork for better claims management and minimizes the chance of errors. How does an effective eligibility verification system benefit patients and providers? Accurate and timely insurance verification clarifies to all parties how bills will be covered (or not) ahead of time. If a claim ends up being rejected, the patient will find themselves with responsibility for more of the bill, the provider will be left uncompensated for services rendered – or both. Clarifying coverage in advance avoids these scenarios. When providers can generate and communicate pre-service patient estimates with confidence, patients can plan for their bills and even make payments before or at the time of service. The financial benefits are clear, but patient satisfaction is also likely to increase: a study by Experian Health and PYMNTS found that patients who received pre-treatment estimates were more satisfied with their care than those who did not. Automated pre-service eligibility checks also improve communication between patients, providers and payers by reducing the manual workload on staff. Instead of spending time checking and fixing errors, staff can focus on helping patients with more complex cases. According to the CAQH, as much as $10 billion could be saved each year by switching to electronic eligibility and benefits verification. How does it help the claims process? In Experian Health’s report on the State of Claims 2022, the most common reasons given for claims being denied included: issues with prior authorizations, provider eligibility, patient information, changing payer policies and services not being covered. Automated eligibility verification helps solve each of these. With fewer errors in the pipeline, organizations can file claims faster and receive payments in a timelier manner. Eligibility Verification accesses up-to-date eligibility and benefits data from multiple sources, generating an instant read-out of a patient’s insurance status. More accurate information increases clean claims rates, accelerates reimbursement and allows providers to forecast future revenue levels more reliably. Staff can view responses in a clear and concise format and receive alerts when follow-ups or edits are required. This sets the tone for a more efficient claims process all around. Proactive and error-free claims management saves staff time that might otherwise be spent on reworking claims and engaging in lengthy disputes with payers. From the patient's perspective, earlier verification can fast-track registration because much of their information is checked before they even arrive for care. Waiting time is reduced because staff benefit from more streamlined workflows. As noted, finding missing coverage gives patients clarity over what they owe, so they’re more apt to pay bills on time. Automation can also be used to connect patients to the appropriate financial support. For example, with Patient Financial Clearance, providers can offer compassionate financial counseling and get patients on the right financial pathway. It improves the patient experience while reducing the risk of bad debt. What does a good insurance eligibility verification system look like? When it comes to choosing an insurance eligibility verification solution, the checklist should include the following features: Compatibility with existing systems and electronic health records - Eligibility Verification accelerates verification and registration by drawing together accurate patient data. And through eCare NEXT®, clients can manage multiple patient access functions through a single interface. Simple methods for updating or changing patient information - User-friendly interfaces allow staff to make changes from any device, as and when new information arises. Integration with patient portals means patients can spot errors themselves, too. And tools such as Registration QA can drive data accuracy by highlighting errors as soon as they occur, both pre-and at the point of service. Rapid results, with patient benefits information readily available when needed - Eligibility Verification confirms patient eligibility and calculates reimbursement estimates with precision. This incorporates CAQH COB Smart® data for enhanced coordination of benefits in relevant transactions. Ability to calculate patient estimates - A verification tool that integrates with automated patient payment estimates ensures patients understand their coverage, co-pays and deductibles before treatment proceeds so that they can plan for their final bills. Integration with pre-authorization tools - For some services, a payer may require the provider to seek authorization before going ahead. An insurance verification solution can flag up where prior authorization is needed to prompt action and prevent delays. Ability to source data from major health insurance carriers, including Medicare - Eligibility Verification connects with nearly 900 payers with advanced search functionality to match patients to current eligibility and benefits data. This can be used alongside an optional lookup service for Medicare beneficiaries to find and validate MBI numbers. Ongoing changes to the health insurance landscape mean that providers must pay close attention to the process of verifying coverage and benefits. Although insurance verification is a small step in patient access, the impact can be felt throughout the patient’s journey and the provider’s revenue cycle. By optimizing for earlier and more accurate insurance verification with workflow automation and advanced data analytics, providers can reduce the risk of denied claims, improve financial performance and protect patient-provider relationships. Find out more about how Experian Health can help healthcare providers streamline their claims process with front-end improvements to verify insurance eligibility, file error-free claims and get paid faster.

“The challenge we sought to overcome by leveraging AI Advantage at our organization was just gaining more insight into how denials originate and what actions we can take to prevent those from happening.” — Skylar Earley, Director of Patient Financial Services, Schneck Medical Center Challenge Starting as a 17-bed hospital more than 100 years ago, Schneck Medical Center now serves four counties in Indiana, with a staff of more than 1,000 employees, 125 volunteers and nearly 200 physicians. The organization’s vision is to deliver excellence, lead transformation and advance health, underpinned by a patient-first philosophy. For the Patient Financial Services team at Schneck Medical Center, reworking denied healthcare claims was often time-consuming and inefficient. Billers tended to prioritize high-value claims, without knowing the probability of reimbursement. They sought a denial management solution that would reduce the risk of denied claims and minimize their impact on the revenue cycle. Solution Schneck worked with Experian Health to test two new denial management solutions that use artificial intelligence (AI) to reduce the likelihood of denials and prioritize rework to maximize reimbursement. The first, AI Advantage™ – Predictive Denials, uses AI to predict claims that have a high chance of being denied, so they can be corrected before the claim is sent to the payer. If a claim review exceeds the suggested threshold for denial probability, an alert is triggered, and the flagged claim is automatically routed to the appropriate biller. The biller investigates the alert to understand what changes are needed. This might include checking insurance eligibility, reviewing coding errors or reviewing authorization status. Once the alert is resolved, the claim can be automatically resubmitted. The second solution, AI Advantage™ – Denial Triage, prioritizes denials based on the potential for reimbursement so staff can focus recovery efforts on the right claims. The triage process starts with identifying between 2 and 10 denial segmentation categories based on likelihood of reimbursement. Schneck chose to identify 5 categories to start. Individual remits are evaluated and automatically assigned to the appropriate category, so they can be routed to the correct specialist. The tools use historical claims data and a continuously learning AI model to detect patterns in payer decisions. Staff can customize denial probability thresholds and segmentation criteria to ensure claims are routed to the correct specialist. The solutions integrate seamlessly with Schneck’s existing claims management system, ClaimSource®, and other health information workflows. Outcome After just six months, AI Advantage helped Schneck reduce denials by an average of 4.6% each month. Corrections that would previously have taken 12 to 15 minutes to rework can now be processed in under 5 minutes. Staff report that the thresholds determined by AI Advantage – Predictive Denials are highly accurate, leading to better decision-making when reworking claims prior to submission. And with AI Advantage – Denials Triage, staff feel confident that they’re focusing their attention on the right segments, rather than wasting time on high-value claims that are unlikely to be reimbursed. Skylar Earley says, “Before, we had no insight into whether we were performing value-added work when we followed up and worked denials. Now we see those percentages.” Learn more about how AI Advantage generates insights to help healthcare organizations reduce time spent working denials and maximize reimbursement.

Healthcare is undergoing a digital revolution driven by artificial intelligence (AI) and machine learning (ML) technology. While some organizations have been slow to adapt, others incorporated new solutions that have helped their organization identify patterns, reduce claim denials, and more. This infographic breaks down common phrases related to artificial intelligence and machine learning so that healthcare organizations can understand what they mean and how they're utilized. Introducing: AI Advantage™ Experian Health is the top-performing claims management vendor, according to the 2023 Best in KLAS: Software and Professional Services report. Experian Health’s ClaimSource® solution, an automated, scalable claims management system designed to prevent claim denials, ranked number one in the Claims Management and Clearinghouse category. With denials and staffing shortages on the rise, an efficient claims management strategy is essential. Experian Health is here to help with AI Advantage™ – a new solution that utilizes true artificial intelligence that proactively helps reduce denials and, when necessary, identifies the best denials to resubmit.
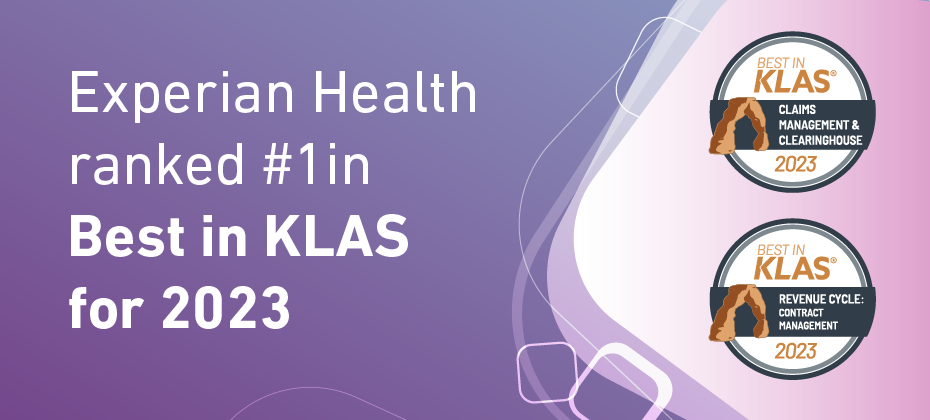
Experian Health is very pleased to announce that it ranked #1 in Best in KLAS, Software and Professional Services, for two segments: #1 in Claims Management and Clearinghouse, for our ClaimSource® claims management system #1 in Revenue Cycle, Contract Management, for our Contract Manager and Contract Analysis product. According to KLAS CEO Adam Gale, “The 2023 Best in KLAS report highlights the top-performing healthcare IT solutions as determined by extensive evaluations and conversations with thousands of healthcare providers. These distinguished winners have demonstrated exceptional dedication to improving and innovating the industry, and their efforts are recognized through their inclusion in this report. Congratulations to all the winning vendors for setting the bar for excellence in healthcare IT! KLAS continues to be committed to creating transparency and helping providers make informed decisions through our accurate, honest, and impartial reporting.” Experian Health’s 2022 State of Claims survey reveals that 47% of providers said that improving clean claims rates was one of their top pain points, with 42% reporting that denials have increased in the past year. Read how Hattiesburg Clinic in Mississippi, which uses both Contract Manager and Analysis and ClaimSource, leverages ClaimSource to automate claims management and reduce denials. Learn more about how ClaimSource and Contract Manager and Contract Analysis can help your healthcare organization.

The consequences of failing to properly verify patient insurance eligibility can wreak havoc on the healthcare revenue cycle. Incorrect patient information, expired policies and missing pre-authorizations can all contribute to denied claims and delayed payments. But with patients bearing a greater responsibility for the cost of care and switching health plans more often, verifying eligibility has become more complex. As patient volumes grow, manual verification processes are increasingly vulnerable to errors. Health insurance eligibility verification software helps providers solve this problem. Few things are more frustrating for healthcare leaders than costly denials that could have been avoided. In a survey by Experian Health, one in three healthcare executives said claims are denied 10%–15% of the time, costing billions of dollars in lost revenue. An automated solution that eliminates errors and reduces denials could pay big dividends across the revenue cycle. This article breaks down the key revenue-boosting benefits of health insurance eligibility verification software: What is eligibility verification? Eligibility verification is the process of checking that a patient’s insurance information is correct and that the services they are seeking are covered under their existing plan. Providers are responsible for verifying the patient’s enrollment status before offering care. Once active enrollment is confirmed, providers will also need to verify the benefits included in the patient’s plan, to be sure that the cost of specific services and items will be covered. This involves the following steps: Checking the patient’s identity and contact information and ensuring that the details on their insurance card match their electronic health record Determining whether the patient’s insurance plan covers the services they expect to receive and that no exclusions apply Confirming that the patient is eligible for proposed services or treatment, for example by ensuring that any pre-authorization or referral requirements have been fulfilled Double-checking that the patient’s coverage is active and that they haven’t exceeded any annual or lifetime limits. "If providers don’t have a full picture of the patient’s payable benefits, deductibles, co-pay thresholds out-of-pocket maximums, and other policy details, they run the risk of non-reimbursement," says Kate Ankumah, Product Manager at Experian Health. "For that reason, these checks should be carried out before a patient’s appointment or procedure, to prevent awkward billing issues and delayed payments. This gives providers peace of mind that they’ll be reimbursed for the services they provide and accelerates patient registration." Carrying out these checks manually can be a time-consuming and laborious process. Staff must check individual payer websites and portals or phone insurance companies to get hold of the necessary information, all while speaking to the patient. Batch processing by medical claims clearinghouses can be a more efficient way of managing eligibility checks, though individual accounts may take longer to clear. What are the benefits of using health insurance eligibility verification software? Given the scale and impact of eligibility checks, many providers turn to insurance verification software to streamline the process and achieve higher levels of accuracy. This offers several benefits to providers and patients: Reduced risk of bad debt - In the world of healthcare claims, errors are expensive. Eligibility verification software can pull from multiple data sources at the click of a button, to give an instant and accurate read-out of a patient’s current insurance details and identity information. Reliable data helps prevent billing errors, thus reducing the risk of disputes with insurance companies. Providers are less likely to bill for services that aren’t covered by the patient’s insurance. Improved patient experience - Billing errors and delays are also major sources of stress for patients. The mismatch between estimated and actual costs is a common complaint. With 3 in 10 patients feeling unable to pay a $500 bill, providers must take steps to provide clarity around the billing process. Automated pre-service eligibility checks help to inform patients of their financial obligations so they can plan accordingly. The software can also support the delivery of tailored, proactive communications to patients, to avoid misunderstandings and queries. Patients are more satisfied with their overall payment experience, while providers see fewer payment delays. Increased revenue - The cost of eligibility errors goes beyond revenue lost through claim denials. If a patient’s insurance information isn’t checked properly, providers bear the financial burden of productivity losses, delayed patient payments, and reputational damage. Eligibility verification software can root out potential mistakes lurking beneath the surface so that claims and communications are correct the first time. By minimizing denials and helping to find missing coverage, this software maximizes reimbursement and accelerates payments. Optimized operations - As noted, using eligibility verification software instead of manual processes can result in significant productivity and efficiency gains. The CAQH reports that electronic eligibility and benefits verification could save medical providers 21 minutes per transaction, amounting to a potential cost saving of nearly $10 billion per year. Automation can release staff from time-consuming calls to insurance companies, reducing their workload and freeing them up to help patients with more complicated needs. This creates a positive patient experience while easing the pressures of staffing shortages. By improving overall revenue cycle management, verification software can increase financial stability. Key features to look for when choosing insurance eligibility verification software By now, most providers will be familiar with automation’s promise of speed, efficiency and accuracy. To fully capture these benefits, providers should choose a software solution with certain key features. Real-time updates allow providers to confirm patient eligibility instantly, without falling foul of any changes to the patient’s coverage that could hamper reimbursement. For example, Experian Health’s Insurance Eligibility Verification solution connects with over 890 payers so providers can access up-to-the-minute eligibility and benefits data. Optimized search functionality increases the likelihood of finding a patient match. An optional Medicare beneficiary identifier (MBI) lookup service finds and validates MBI numbers, ensuring timely reimbursement, which is especially important as COVID-19 funding comes to an end. Next providers should look for a user-friendly interface. Insurance Eligibility Verification adapts responses from multiple payers so that registrars can access patient details in a consistent format, regardless of the original layout. Customizable alerts notify staff when action is needed. A major advantage of automated solutions lies in the possibility for more detailed reporting and analytics. A tool that synthesizes performance data can provide at-a-glance status updates for senior managers and help staff identify opportunities for improvement. Similarly, providers should look for a tool that fits neatly with their existing electronic systems and interfaces, to fully leverage data analytics and streamline operations. Integration with electronic health records can fast-track verification and registration by providing a single source of truth regarding patient information. Existing Experian Health clients will be able to access Eligibility Verification through eCare NEXT®, providing a single interface from which to manage several patient access functions. Automated verification: a smart investment? Rachel Papka, Director of Health Systems at Steinberg Diagnostic Medical Imaging says Experian Health’s eligibility products have helped her team to validate patient coverage in under 30 seconds: “The Eligibility and eCare NEXT piece allows us to see if the patient is eligible with the insurance they just presented quickly and in real-time – in under 30 seconds. As I'm facing the patient, I'm not hiding behind a phone. I'm not trying to log on to a different website. I'm literally interacting with the patient at the time of service with the eCare NEXT platform, and it's telling me their deductible or coinsurance or co-payments, and I can accurately collect from that patient right there. And it directly writes into my electronic medical record, so users only need to use one system.” For the 3 in 4 healthcare executives who said reducing denials was their top priority, automated insurance verification could be a wise investment. Find out more about how Experian Health’s health Insurance Eligibility Verification software could hold the key to streamlined claims management, fewer denials and faster cash flow.

Hattiesburg Clinic is Mississippi’s largest multispecialty clinic with over 450 physicians serving 19 counties. Claims management, patient collections and payer contract management are handled by the clinic’s Financial Services Department, which includes around 70 staff members. Challenge Hattiesburg Clinic in Mississippi sought to improve financial performance in the wake of the COVID-19 pandemic by focusing on reducing claim denials. The Financial Services Department had been hit by staffing shortages, which affected financial results. A more efficient digital claims management solution would attract and retain a high-performing virtual team, while supporting the shift away from existing paper-based systems. To submit more clean claims the first time, the Department set specific goals to: meet or exceed Epic benchmarks for primary denials maintain accounts receivable (AR) days at 42 or less process secondary and tertiary claims without waiting for the primary electronic remittance advice (ERA) to be posted. Solution Already impressed with Experian Health’s Contract Manager and Eligibility solutions, the Department chose another Experian product, ClaimSource®, to help reduce denials. Loretta McLaughlin, Assistant Director of Financial Services, said she was confident ClaimSource was a good candidate for the clinic’s claims platform: “ClaimSource seemed like the right fit for the department’s goals. The platform’s ability to customize edits, along with the level of customer support available, really set the solution apart from the alternatives.” ClaimSource uses scalable automation to prioritize claims, payments and denials. This allows staff to use their time as efficiently as possible, by working on the highest-impact accounts first. Using customizable edits and extensive national and local payer edits, it checks each claim for inconsistencies before the claim is submitted. ERA data is automatically integrated into Epic so that staff can check a claim’s status quickly and easily. With real-time reporting, staff gets insights from across the entire claim lifecycle to improve performance. Outcome The ability to integrate customizable edits was a big advantage for the clinic. They now have over 90 custom edits that help eliminate time-consuming errors, reduce denials, and allow staff to focus on the right accounts. As a result, Hattiesburg Clinic has achieved a 6.1% primary denial rate, which exceeds the Epic Financial Pulse benchmark. Despite staffing shortages, they’ve been able to accelerate receivables. They’re also seeing accelerated cash flow, now they can pursue claims from secondary and tertiary payers without awaiting the outcome of primary claims adjudication. ClaimSource is also creating a better staff experience: the tool eliminates the need for claims to be printed, so staff can work from any location. Now, over 50% of the team work from home. Thanks to automated workflows, output has been consistent despite a reduced workforce. Being able to submit clean claims the first time has a positive impact on AR days as well as staff workload. Loretta McLaughlin says: “Through ClaimSource’s automation and level of quality work, we have had to do less manual intervention.” To build on this success, the team intends to explore further opportunities to use automation to improve productivity. Options include automatically generating patient estimates, automating bad debt and refund workflows, and allowing patients to verify insurance eligibility through their patient portals. Find out more about how ClaimSource helps hospitals, health systems and physician groups reduce denials, protect profits and increase productivity through automated and scalable claims management.

In 2009, processing claims was listed as the second greatest contributor to “wasted” healthcare dollars in the US, at an estimated $210 billion. A decade later, that amount was estimated at $265 billion. Today, healthcare providers are still grappling with denied healthcare claims, with both challenges and solutions accelerated by the pandemic. To put the scale of operational and delivery changes into perspective, Experian Health recorded well over 100,000 payer policy changes for coding and reimbursement between March 2020 and March 2022. The implications for claims processing are immense, which is why healthcare providers need to reevaluate their denial management strategies and invest in new technology that can help increase reimbursements. In June 2022, Experian Health surveyed 200 revenue cycle decision-makers to understand how they feel about the current situation. What are the priorities of those on the front line of denials management? And how can technology contribute to improvements? This article breaks down the key findings. Takeaway 1: Denials are increasing and reducing them is priority #1 30% of respondents say denials are increasing by 10-15% Nearly 3 out of 4 respondents say that reducing denials is their top priority For most respondents, claims management is more important now than it was before the pandemic, because of payer policy changes, reimbursement delays and increasing denials. Respondents attribute this to insufficient data analytics, lack of automation in the claims/denials process and lack of thorough staff training. When it comes to improving denial rates, staffing seems to be the greatest challenge. More than half of respondents say staff shortages are slowing down claims submissions and hampering efficiency. Shrinking offices mean there is less staff to handle the growing volume and complexity of claims. It’s no surprise, then, that around 4 in 10 respondents are also concerned about keeping up with rapidly changing payer policies and keeping track of pre-authorization requirements. Providers recognize that technology can help reduce denials while easing the burden on staff. A tool like ClaimSource manages the entire claims cycle using customizable work queues that make it easy to prioritize accounts, saving staff time and avoiding the errors that lead to denials. This also incorporates payer edits to ensure that claims are clean before being submitted to the payer. And if claims do end up needing further attention, Denials Workflow Manager eliminates time-consuming manual processes and allows providers to attend to high-risk claims quickly, so there’s less chance of delayed reimbursement. Takeaway 2: Automating denials management in healthcare is critical 52% of respondents upgraded or replaced previous claims process technology in the last 12 months 51% are using robotic processes, including automation, but only 11% are using artificial intelligence Prior to the pandemic, automation was sometimes perceived as a threat to jobs. But with changing employment patterns and evidence of the broader benefits of automation, attitudes are shifting. Automation can make life easier for staff by removing manual tasks to allow them to focus on other priorities. It speeds up the healthcare claims processing workflow, reduces the risk of errors, and enables better communication between providers, patients and payers. Providers recognize that automation drives more efficient claims management. The survey revealed that 45% of respondents turned to automation to keep track of payer policy changes, 44% had automated patient portal claims reviews, and 39% had digitized patient registration in the last year. Automation supports all stages of the claims management process, from auto-filling patient data during registration, to generating real-time claim status reports for back-office staff. Payer authorizations were a common challenge for providers, and a perfect fit for automation. Experian Health’s Prior Authorizations solution eliminates the need for staff to visit multiple payer websites, automates inquiries, and offers real-time updates on pending and denied submissions so staff knows when to intervene. Takeaway 3: Providers are searching for denial management solutions that will achieve the greatest ROI 91% of those likely to invest in claims technology say they will replace existing solutions if presented with a compelling ROI The majority of providers may be on the lookout for better claims management solutions, but they vary in how they measure ROI. Predictably, one of the most common metrics is how much staff time can be saved, with 61% concerned with hours spent appealing or resubmitting claims, and 52% looking at time spent reworking claims versus reimbursement totals. Rates of clean claims and denials were also popular metrics, at 47% and 41%, respectively. Using Denials Workflow Manager and ClaimSource alongside additional claims management solutions like Claim Scrubber and Enhanced Claim Status can deliver an even stronger performance against the above metrics. Each solves a specific challenge within the claims management workflow, but when used together, the ROI is multiplied. Overall, there’s optimism that digital technology and automation can help healthcare providers improve claims and denial management and reduce the amount of “wasted” dollars. This survey shows that providers are keen to grasp the opportunities offered by automation to optimize the reimbursement process and get paid sooner. Download the report to get the full results on the State of Claims 2022, and discover how Experian Health can help organizations with their denial management strategies.

When it comes to medical coding and billing, accuracy is everything. Even the smallest error can result in a claim being bounced back by the payer, causing delays and missed revenue opportunities. Coding requirements change frequently, and with denials totaling billions of dollars per year, providers can’t afford to risk under- or over-coding or relying on outdated codes. Automation and software-driven solutions can uncomplicate the complex world of medical coding. Getting claims right the first time accelerates the adjudication process, leading to faster and higher reimbursements. Providers can make more reliable financial forecasts, avoid losing time reworking rejected claims, and give patients greater clarity about what they’ll owe. For this reason, providers should brush up on medical coding and billing best practices to improve claims management and maximize reimbursements. Here are 7 areas to focus on: 1. Stay up-to-date with coding changes Medical codes convert information about the patient’s healthcare encounter into an electronic format that payers use to adjudicate claims for reimbursement. If a claim includes outdated, incorrect or missing codes, then it will be denied. The most common medical coding systems include: International Classification of Disease 10th edition (ICD-10) codes: these codes denote the patient’s diagnosis or condition. The 11th version was published in January 2022, and while the implementation timeline in the US remains unclear, providers will need to be ready to adapt. Current Procedural Terminology (CPT) codes: Where ICD codes describe the patient’s symptoms, CPT codes record their treatment. If there’s a discrepancy between diagnosis and treatment, the claim is likely to be denied. Healthcare Common Procedure Coding System (HCPCS) codes: the Centers for Medicare and Medicaid Services (CMS) use these to apply CPT codes to procedures, services, products and equipment offered to Medicaid and Medicare patients and those covered by private insurance. These codes are constantly being revised and are often recycled, so coders must pay close attention to avoid errors. National Drug Code (NDC): claims need to include NDC codes when the patient is taking prescribed or over-the-counter medications. The NDC directory is updated daily. Diagnosis-Related Group (DRG) codes: these combine ICD and CPT codes to determine the final amount that a hospital can be reimbursed. CMS assigns annually calculated weightings to DRGs based on severity and length of illness, treatment trends and other factors. There are also multiple coding directories for different specialties, such as dental care, mental health and patients with disabilities. With hundreds of thousands of constantly-changing codable terms to consider, medical coders face a daunting task. In the past, coders would rely on manual coding directories to find the right codes, but today, most use digital encoders and digital coding libraries to generate electronic codes. For example, Experian Health’s claims management software integrates government and payer edits so that no changes to coding requirements are missed. Each patient encounter can be processed in real time and incorrect codes can be flagged before the claim is submitted. 2. Automate the claims management process to increase medical billing and coding accuracy Manually matching each patient encounter to a specific set of codes is time-consuming and vulnerable to errors. Software programs improve the process by analyzing unstructured clin constantly-changing codable terms ical charts and notes to draw out information relevant to the claim. They can cross-reference multiple coding directories in an instant to identify the correct code. They also compile data in standardized, interoperable formats so information can be exchanged between coding and billing teams, clearinghouse staff and payer systems with ease. While some of the output generated by machine learning systems still needs to be checked by human eyes, automated solutions drastically reduce the burden on staff and ensure greater accuracy. With automated claims management, medical coding and billing teams can optimize their workflows, submit cleaner claims, and get insights into the root causes of denials. Case study: see how Summit Medical Group Oregon – Bend Memorial Clinic used automated claims management technology to achieve a primary clean claims rate of 92%. 3. Eliminate workflow inefficiencies to save time According to the Council for Affordable Quality Healthcare (CAQH), automation could save more than an hour of staff time for every three claim status checks. Automation frees up staff to focus on the highest priority tasks that require a human touch. Fewer errors mean less time spent on reworking denied claims. And if claims are processed more quickly, this means that they reach the payer adjudication stage sooner which ultimately will result in faster payments. The medical coding and billing process takes anywhere from a week to a few months, so every hour saved makes a difference. To this end, Enhanced Claim Status monitors how claims are progressing through the claims adjudication process, reducing the amount of time staff need to spend interacting with payers. It eliminates manual follow-up and allows teams to address pending, returned, denied and zero-pay transactions before the Electronic Remittance Advice and Explanation of Benefits are processed. Worklists are generated based on actionable data so staff can work more productively, and claims get settled sooner. 4. Customize claims edits to your specifications One way to drive up medical coding accuracy is to use customized claims edits. Some claims management software solutions only apply updates using universal claim edits or using groups of edits. This doesn’t work for large medical groups that need to cover multiple combinations of payer, specialty and geographical edits. Since no two payer policies are the same, claims edits would need to be checked manually to make sure nothing has been missed. Experian Health’s claims management software solves this by incorporating government and commercial edits alongside client-specific customized edits. Providers can keep pace with changes and capture the requirements of all reimbursement policies that are relevant to a particular claim. For example, ClaimSource runs front-end claims editing to coordinate federal, state and commercial payer edits together with customized provider edits to avoid coding errors. Similarly, ClaimScrubber automatically reviews and adjusts claims, helping medical groups streamline claims submissions. 5. Upgrade record-keeping technology to maintain medical billing and coding accuracy If patient records are peppered with typos and outdated contact information, then it’s highly likely that errors will be inherited on claims forms. A fifth of patients have spotted errors in their health records, including incorrect details about diagnoses, medications and test results. Preventing these errors is key to maintaining medical billing and coding accuracy. Interoperable electronic patient records protect against inaccuracies by creating a single, complete record for each patient. With a tool such as Universal Identity Manager, patient data is matched against multiple data sources to verify that the record is complete and accurate. Staff can have confidence that all information held on a patient will be taken into account when their medical encounters are coded, and avoid coding discrepancies that can occur when a patient’s treatment doesn’t seem to match their diagnosis. 6. Double-check claims before submitting Running a line-by-line review of each claim before it’s submitted means errors can be found and fixed before they result in financial losses. This would be a painstaking task to do by hand, but with tools such as ClaimSource and ClaimScrubber, hospitals and medical groups can audit claims automatically to check for coding discrepancies or missing patient information. A streamlined claims cycle benefits payers and patients too. Payers can adjudicate accurately coded claims more quickly without pushing them into a queue for manual review, and patients get earlier clarity about how much they’ll owe. 7. Audit the claims management process to spot medical coding inaccuracies Finally, it makes sense to undertake regular audits of the medical coding and billing procedures to weed out any recurring issues. While a coding audit will focus on coding accuracy and compliance, a billing audit can investigate the systems and processes involved in everything from patient eligibility verification to patient collections. This helps uncover recurring issues with under- and over-coding, use of redundant and retired codes, non-compliance and poor documentation. Again, maintaining robust, quality data and records will make this process easier. Partnering with a single, trusted vendor to deliver an end-to-end claims management solution can help achieve this. Find out more about how Experian Health’s automated claims management solutions can help healthcare organizations maintain medical billing and coding accuracy, drive down denials and create a more predictable revenue cycle.