
“Reducing denials upfront would improve our revenue, which could be channeled into current and future investments that support our mission.”
—Joshua Gayman, Revenue Cycle Manager at UT Medical Center
Challenge
The University of Tennessee Medical Center (UT Medical Center) is a leading 710-bed acute care hospital with a rich history of exceptional patient care and award-winning services. During the pandemic, the hospital faced revenue losses of around $45 million that put serious strain on its capacity to invest in bigger and better facilities. UT Medical Center needed to find a strategy to recover some of this revenue by reducing claim denials at the point of patient registration.
UT Medical Center relied on eligibility checks that often missed errors in patient registration, resulting in increased claims denials, costly reworks, and wasted staff time. The hospital urgently needed a solution to help staff identify and resolve potential patient registration errors in real time to prevent denials before they occur. Finding a more efficient way to capture accurate patient and benefits data would be essential. Proactively preventing claim denials would provide the hospital with a much-needed boost in cash collections and free up staff to focus on patient care.
Solution
To address its claims denials challenge, UT Medical Center partnered with Experian Health and implemented Registration QA, a solution designed to find and fix registration errors upfront. Now, when patients first arrive, front-end staff enter their data to verify insurance. If Registration QA finds an error, it alerts staff in real-time so they can resolve it within 72 hours. Alongside more than 400 alert rules curated by Experian Health, UT Medical Center also built custom alerts based on the organization’s specific requirements, using demographics and benefits data.
The tool easily integrates with existing workflows, and its configurable dashboard gives UT Medical Center Management detailed insights into department performance and allows staff to track trends and identify areas for improvement. This proactive approach to correcting errors significantly reduces the risk of downstream denials and helps patient registration staff take proper corrective actions for their errors without management intervention. More accurate patient registration is also better for patients, as fewer errors make for a smoother intake experience.
Outcome
UT Medical Center successfully optimized patient registration by using Registration QA to identify registration errors before and at the point of service, reducing denials and boosting revenue.
In the 12 months after implementing Registration QA, UT Medical Center saw the following results:
- Now that registration errors can be identified before and at the point of service, UT Medical Center has seen initial denials drop from an average of $5 million per month in 2022 to just $1.7 million in 2023, representing a 66% decrease in average monthly initial denials value.
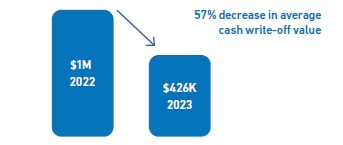
- Cash write-offs also decreased, dropping 57% from an average of $1 million to just over $400K, helping the organization keep bad debt low.

Gayman notes that UT Medical Center’s partnership with Experian Health was central to its success. Experian Health shared the organization’s vision and provided weekly support to help realize it. They developed a customized curriculum to make sure staff were confident using Registration QA and offered insights into what was happening more widely in the industry, so UT Medical Center’s team could benchmark their performance against similar organizations.
Thanks to these savings, the hospital can increase its capacity to invest in new projects and deliver operational excellence, while improving patient satisfaction.
Find out more about how Registration QA helps healthcare organizations minimize denials and increase cash flow through accurate patient registration.


