Artificial intelligence (AI) is changing the healthcare industry. From disease detection to chatbots, AI is having a significant impact on the way healthcare providers operate and deliver care to patients. Additionally, AI is transforming the revenue cycle management process by automating tasks, such as claim denials management. By leveraging AI tools, healthcare providers can reduce the time and resources required for manual claims processing, ensuring that claims are paid faster and with greater accuracy.
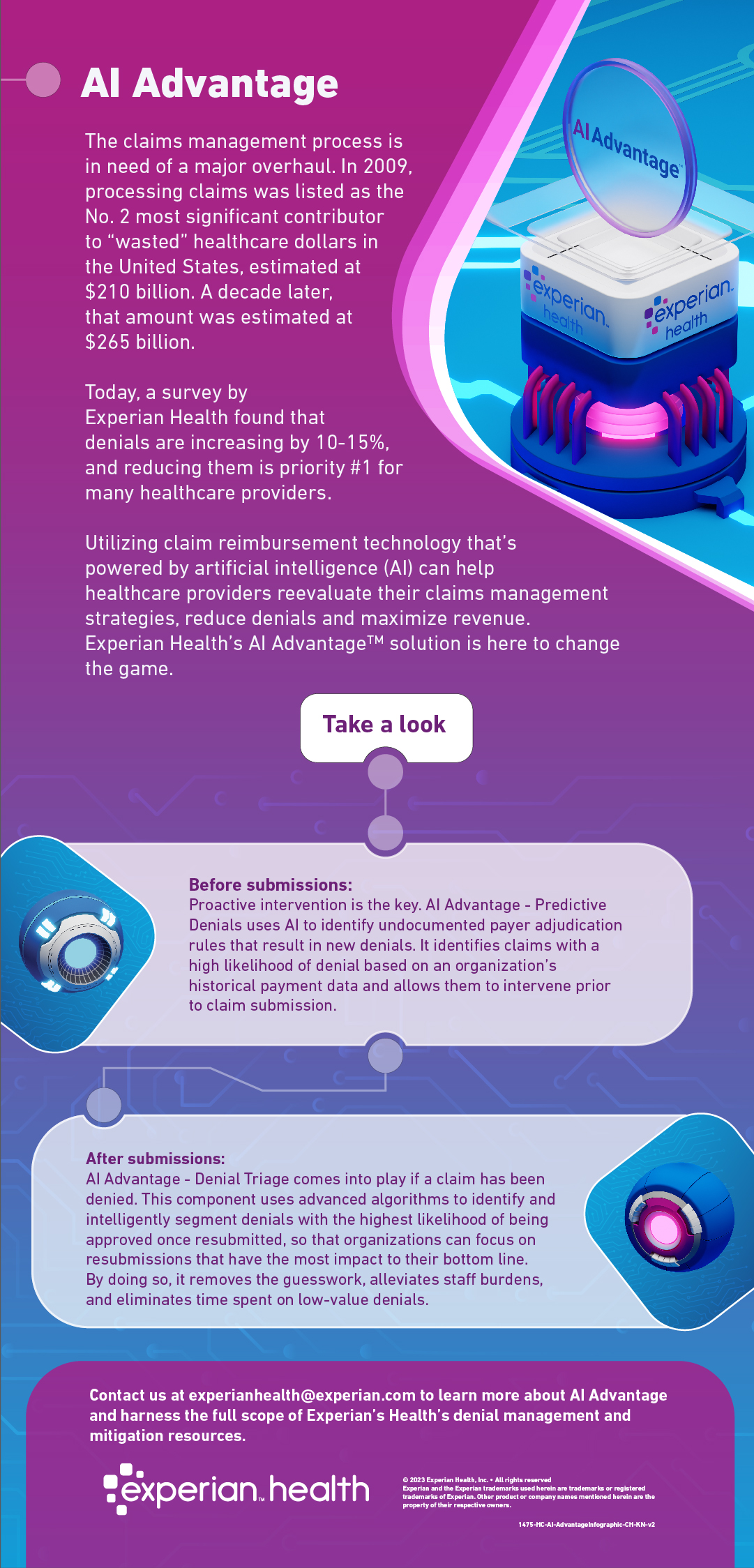
As claim denials continue to rise by 10-15%, healthcare organizations continue to grapple with the adverse effects on their finances. That’s why Experian Health created AI Advantage™ – an innovative solution that helps providers with better claim denial management. The first component, AI Advantage – Predictive Denials, proactively identifies claims that are at high risk of being denied, so providers can edit the claim prior to submission. The second component, AI Advantage – Denial Triage, steps in after claims have been denied to identify those with the highest potential for reimbursement.
Schneck Medical Center is one example of a healthcare organization that has seen significant results from implementing AI Advantage. After just six months, they successfully reduced denials by an average of 4.6% each month. Corrections that would previously have taken their organization 12 to 15 minutes to rework could now be processed in under 5 minutes.
With AI Advantage, healthcare organizations can improve their claim denials management processes, increase efficiency, and reduce administrative costs. The solution’s ability to prevent and reduce claim denials in real time can help healthcare providers maximize revenue while delivering high-quality patient care. As healthcare organizations continue to face mounting financial pressures and staffing shortages, AI-powered solutions will be increasingly important in helping them navigate these challenges and achieve long-term success.
Learn more about how healthcare organizations can begin their journey towards improving efficiency and reducing claim denials with AI Advantage.